Understanding Hit-and-Run OCD: Causes and Treatment
Have you been diagnosed with hit-and-run OCD, or are you simply curious as to what it might be? Today, we look at the science behind it and its severe impact on motorists.

Despite the challenges that hit-and-run OCD presents, understanding this condition can help those afflicted manage its symptoms with the right treatment plan.
In this blog post, we will explore what causes hit-and-run OCD, provide brief overviews of common symptoms, and recommend effective treatments that have been proven successful in treating obsessive-compulsive disorders like this one.
What Is Hit-and-Run OCD?
Hit-and-run OCD is a subset of harm OCD characterized by an intense fear of accidentally hitting, injuring, and potentially killing a pedestrian, animal, or object while driving, even if there is no evidence to suggest that this has happened.
The intrusive thoughts associated with hit-and-run OCD can be so vivid and unpleasant that they often provoke feelings of distress.
People with this OCD type may obsess about running someone over and not noticing, hitting a parked car and not noticing, causing a car accident and not realizing it, and so on. It may even go as far as creating a false memory, remembering something that did not happen.
These worries can lead those suffering from this disorder away from public places, such as driving or gathering in crowded spaces – all out of fear that their unchecked imaginations could become a reality.
Likewise, it may lead to an onset of compulsive behaviors, including filing police reports, monitoring emergency vehicles, repeatedly apologizing, seeking reassurance, and even driving around for hours in search of the person they believe they may have accidentally hit.
Overall, individuals suffering from hit-and-run OCD tend to experience paranoia around accident scenes. Often, the burden may be so great that it forces them to quit driving, which will negatively impact their private and social life.
What Causes Hit-and-Run OCD?
Given the complexities of this disorder, one thing is certain: there is no one source responsible for hit-and-run OCD. Hit-and-run OCD results from multiple factors based on scientific evidence.
People suffering from any type of OCD have a different brain structure and function than other people without this condition, something science refers to as neurodivergence.
In the case of OCD, the amygdala, the part of the brain responsible for processing memory, decision-making, and emotional responses such as fear, aggression, and anxiety, is put on high alert, indicating the presence of a threat even when there is none.
Research suggests that individuals with hit-and-run OCD tend to have an imbalance in serotonin and dopamine levels. These neurotransmitters are vital as they reduce anxiety, depression, lethargy, and more.
There is also the genetic side at play. According to statistics, 1 out of 4 people living with OCD has a family member with OCD. Still, it’s important to note the nuances regarding being genetically predisposed to certain conditions.
People can get OCD without being genetically predisposed, while those who are genetically predisposed may not have this mental condition.
There’s also the behavioral factor to consider. However, this is a confirmation of the disorder rather than a cause – the manifestation of hit-and-run OCD is in the obsessive and compulsive behaviors.
Overall, it’s difficult to pinpoint what causes a person to develop a specific type of OCD. OCD goes against a person’s values, and in the case of hit-and-run OCD, the individual’s apprehension stems from not wanting to cause any road accident.
Hit-and-Run OCD Treatment
Regarding hit-and-run OCD treatment, medication and psychotherapy are the proven methods that work. Here is an outline of some of these methods.
#1 Cognitive behavioral therapy (CBT) with exposure and response prevention (ERP)
CBT with ERP is considered the gold standard of OCD treatments. Cognitive behavioral therapy emphasizes exploring the relationship between thoughts, feelings, and behaviors. Exposure and response prevention reduce obsessive-compulsive behavior by gradually introducing a person to their anxiety-provoking thoughts or situations.
In essence, this treatment requires the patient to expose themselves to intrusive thoughts or sensations, allowing them to engage in their compulsive behavior as a sort of “desensitization” process.
After repeatedly experiencing these thoughts or feelings, the patient then learns to refrain from engaging in the compulsions, which are usually paired with unwanted mental images.
With these two interventions combined, cognitive restructuring is used to weaken strict beliefs associated with the disorder by teaching patients more productive thinking patterns that can help reduce the presence of distressing thoughts related to hit-and-run OCD.
These techniques help an individual be better equipped to confront problematic situations and make behavioral changes that can ultimately alleviate symptoms of the condition.
By working together through this therapeutic process, clinicians and their patients can find relief from this condition and lead more meaningful lives.
There are other ways to go about CBT; good examples are mental health apps and journals.
It is important to note that while apps may be a useful tool for some individuals with OCD, it is not a standalone treatment and should not be used in place of professional care.
If you are seeking treatment for OCD, speak with a mental health professional who can help you determine the best treatment for your specific needs.
#2 Acceptance and commitment therapy (ACT)
This is another scientifically praised method used in treating OCD spectrum disorders. Acceptance and commitment therapy aims to help individuals accept their thoughts and feelings rather than trying to control or eliminate them.
This method enables OCD sufferers to restructure the relationship between their thoughts, feelings, and reality, giving them better control over their mental state.
It also involves committing to action that is consistent with one’s values, even in difficult thoughts and feelings. ACT has been found to be effective in treating OCD and has been shown to reduce symptoms and improve quality of life.
According to research, individuals with OCD who received ACT in addition to medication reported significant reductions in OCD symptoms and an improvement in quality of life, even those who dropped out of the study mid-trial experienced the same positive effects.
However, the effectiveness of ACT in the treatment of OCD can vary from person to person. Some individuals may find ACT a particularly helpful treatment approach, while others may not experience the same benefits.
It is also worth noting that ACT is typically used in conjunction with other treatments, such as medication or ERP. The combination of treatments that is most effective for a particular individual may depend on their symptom severity and specific needs.
#3 Medicine
According to a study, 70% of people living with OCD respond to some form of medication. However, there is a limit to the said response.
So far, there exists no pill that cures OCD completely, and therapy still remains the main treatment option. On the whole, these OCD medications help ease the stress associated with ERP therapy, and this increases the chances of success.
It is important to note that OCD medication does not come as one-pill-fits-all medicine, and individuals with OCD tend to respond differently based on their genetics. In fact, there are records of individuals with OCD who do not respond at all to these medicines.
Regarding medications, serotonin-specific reuptake inhibitors (SSRIs), a class of antidepressants that increase serotonin levels, are the primary drug class used. Some examples of SSRI drugs include:
-
- Fluoxetine (Prozac)
-
- Sertraline (Zoloft)
-
- Celexa
-
- Paroxetine (Paxil)
-
- Fluvoxamine (Luvox)
-
- Escitalopram (Lexapro)
An OCD therapist may also include serotonin-norepinephrine reuptake inhibitors (SNRIs), as they increase serotonin and norepinephrine levels. Examples of SNRIs include:
-
- Venlafaxine (Effexor)
-
- Duloxetine (Cymbalta)
-
- Desvenlafaxine (Pristiq)
-
- Milnacipran HCl (Savella)
-
- Levomilnacipran (Fetzima)
Another drug that has gained clinical grounds is Anafranil (Clomipramine). Unfortunately, while its potency in treating different types of OCDs is on the high side, it comes with some of the strongest side effects among other OCD drugs.
Aside from the different OCD drugs, doctors have begun to prescribe off-label drugs. The drawback is that these drugs do not carry FDA approval as treatment options for OCD. However, they help treat other conditions, carrying the required FDA approval.
Among the list of these off-label drugs are the following:
-
- Xanax
-
- Risperdal
-
- Haldol
-
- Zyprexa
-
- Tramadol
-
- Seroquel
-
- Buspar
-
- Abilify
-
- Valium
-
- Namenda
-
- Namenda
-
- Ketamine
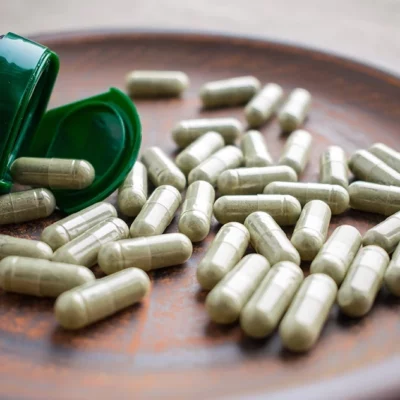
Over the years, some people have resulted in using over-the-counter supplements (nutraceuticals) as a treatment for their hit-and-run OCD. Hit-and-run OCD supplements include:
-
- Probiotics
-
- NAC
-
- CBD
-
- Resveratrol
-
- Glycine
-
- Milk thistle
-
- Borage
-
- Curcumin
-
- St. John’s Wort
Still, there is little scientific backing that confirms the effectiveness of these supplements in treating OCD. Yet, there are a lot of anecdotal reports declaring their efficacy.
#4 Transcranial magnetic stimulation (TMS)
Another new yet effective treatment option involves the use of a magnetic field to regulate the areas of the brain involved in OCD.
Transcranial magnetic stimulation (TMS) is a non-invasive procedure that alters the activity of neurons in the magnetically stimulated area of the brain.
With this procedure, a magnetic coil is connected to the scalp, and an electric pulse generator is attached to it. This couple induces an electric current fed directly to the designated brain area through electromagnetic induction.
Neuromodulation is also increasing in popularity as a treatment for anxiety, PTSD, and depression, and this might prove useful in treating OCD.
What Are the Symptoms of Hit-and-Run OCD?
For starters, it’s important to note that hit-and-run OCD symptoms vary across individuals – a common trend with OCD spectrum disorders. While complexities may stem, some symptoms remain fairly common, including:
-
- Intrusive thoughts about causing harm
-
- Stress and anxiety
-
- Repeated apologizing
-
- Paranoia about accidents or driving
-
- Driving around for hours in search of the person they are convinced they hit
-
- Avoiding crowded areas and traffic
-
- Monitoring police accident reports and ambulance radio calls
Difference Between Hit-and-Run OCD and Driving Anxiety
While hit-and-run OCD leads to driving anxiety, it is not the sole cause of this problem. In fact, cases of driving anxiety might be completely unrelated to hit-and-run OCD. Hit-and-run OCD involves experiencing a shower of intrusive thoughts, transcending to obsessive and compulsive behaviors.
With driving anxiety, you want to watch out for two other forms: panic disorder and agoraphobia. Panic disorder goes hand in hand with a fear of specific bodily sensations, including heart attacks, going unconscious, and dizzy spells.
On the other hand, agoraphobia causes you to fear and shy away from places or situations that cause you to feel entrapped.
The only way to determine if you suffer from driving anxiety or harm OCD is to get evaluated by a professional, and just like with hit-and-run OCD, there exist ways to deal with panic attacks while driving.
5 Tips on How to Stop Hit-and-Run OCD
There are some ingenious ways to help stop your hit-and-run OCD attacks. These self-help tips give you better control over your symptoms and their influence. Some of these include:
-
- Identify your triggers: This is, perhaps, the most important aspect in controlling the influence your hit-and-run OCD has over you. By identifying the places and events that trigger your OCD, you can avoid making your OCD worse by staying away from such areas.
-
- Take it slow: Instead of succumbing to the influence of your OCD and quitting driving, you can map out driving routes with less traffic, as this would generally reduce your stress and anxiety. Once you are used to the feeling of driving freely, you can move on to more crowded areas.
-
- Practice mindfulness: This involves paying attention to your intrusive thoughts and feelings in a non-judgmental way and can help you learn to respond to your obsessions and compulsions in a more balanced and healthy way.
-
- Live a healthy lifestyle: It is common knowledge that living a healthy lifestyle transcends both physical and mental well-being. So, make sure to eat a balanced diet, exercise regularly, avoid alcohol, drugs, and other intoxicants, and prioritize sleep.
-
- Join a support group: Joining a support group will help greatly with hit-and-run OCD. You can share your problems with other OCD sufferers, meet OCD specialists, and access effective treatment.
What Consequences Can Hit-and-Run OCD Have?
A very real potential consequence of this condition is the danger presented by a hit-and-run car accident. The inability to stop intrusive thoughts or obsessing over certain tasks can cause a distracted driver to make decisions that can lead to an unfortunate car accident.
Likewise, the sufferer may become increasingly anxious, potentially leading to depression and anxiety-related disorders. They might also further isolate themselves as they try to avoid situations where they fear making a mistake that could lead to the repercussions of their mistake being discovered.
In extreme cases, individuals with OCD might even become suicidal as the pressure from their own irrational thinking intensifies.
FAQs
No, hit-and-run OCD is not a common type of harm OCD. Hit-and-run OCD still counts as a serious problem.
Your best bet to overcoming driving OCD is any of the clinically endorsed treatment methods. However, some self-help tips make living with this OCD a lot easier.
The best help you can offer a hit-and-run OCD sufferer is encouragement regarding seeking effective ways to manage their condition.
Conclusion
So, there we have it. A comprehensive guide to hit and run OCD. If you or someone you know suffers from this condition, do not hesitate to seek help. With the right treatment, anyone can overcome their compulsions and live a healthy, happy life.















































 Select your language:
Select your language: