Diabetes 101: Types, Symptoms, and Healthy Living Tips
Your guide to diabetes, from types and causes to management and lifestyle tips.

Often called the silent killer, diabetes mellitus is a disease that affects communities worldwide. Genetics, diet, lifestyle choices, and other factors can contribute to this condition, and it’s important to gain a deeper understanding of its risk factors.
Receiving a diabetes diagnosis can be difficult. You may have a lot of questions. If you are dealing with diabetes, keep reading as this article delves into the topic, covering everything from types and symptoms to living with your diagnosis.
Diabetes: What Is It?
Diabetes, or diabetes mellitus, is a chronic metabolic disease that occurs when the body either can’t make enough insulin or can’t use insulin properly, resulting in abnormally high blood sugar levels. A progressive disease, untreated diabetes can eventually cause serious damage to the blood vessels, nerves, eyes, kidneys, and heart.
According to the National Diabetes Statistics Report, 37.3 million people in the United States are living with diabetes – a whopping 11.3% of the population. Alarmingly, 8.5 million of these people remain undiagnosed.
Types of Diabetes
A diabetes diagnosis means you have one of three main types of diabetes, which includes type 1, type 2, or gestational diabetes. The type you have determines how best to manage the condition.
#1 Type 1 diabetes
Type 1 diabetes is a lifelong autoimmune disease where there is too much glucose in the bloodstream. It occurs when your pancreas doesn’t make insulin. Since you can’t survive without insulin, type 1 diabetes is a life-threatening disease. If you have the type 1 variety, you must use insulin daily to live.
#2 Type 2 diabetes
Like type 1 diabetes, high blood sugar levels characterize type 2 diabetes. However, type 2 diabetes is a metabolic condition that occurs when your pancreas doesn’t make enough insulin to control your blood sugar or when your body doesn’t respond to insulin properly.
Of the 37 million Americans with the disease, approximately 90–95% have type 2 diabetes, making it the most common type.
#3 Gestational diabetes
Gestational diabetes arises during pregnancy in women who don’t already have the disease. It happens when the body is unable to make enough insulin during pregnancy to control blood glucose, causing levels to rise.
Untreated, gestational diabetes can cause complications in pregnancy, but it is controllable and blood sugars usually return to normal after giving birth.
#4 Prediabetes
Prediabetes is not a diabetes diagnosis but can be a precursor to type 2 diabetes. It indicates that blood sugar levels are abnormally high but not enough to warrant a diabetes diagnosis yet.
It’s important to manage prediabetes to prevent its progression. You can avoid type 2 diabetes if you take the right steps to manage your blood sugars, such as losing excess weight and engaging in regular physical activity.
What Causes Diabetes?
Scientists are still trying to clarify the exact cause of diabetes. Although all result in excess sugar levels in the bloodstream, there are reasons behind diabetes that differ depending on the type.
There are also known diabetes risk factors that contribute to its development and encourage diabetes complications.
Type 1 diabetes
You get type 1 diabetes when your pancreas doesn’t make insulin, a naturally occurring hormone the human body needs to regulate blood glucose. It helps blood glucose enter the cells, where it converts into energy and signals the liver to store any extra for later.
In type 1, the immune system attacks itself, wrongfully destroying beta cells in the pancreas that produce insulin. The exact cause is unknown, but the evidence points to genetics and viral infections as possible triggers.
Type 2 diabetes
With type 2 diabetes, the pancreas is still producing insulin. However, there is deficient insulin production to maintain healthy blood glucose levels, or the cells don’t respond to and use insulin properly. This is known as insulin resistance.
Genetics and lifestyle choices like poor diet, smoking, and being physically inactive can contribute to type 2 diabetes.
Gestational diabetes
A family history of diabetes can increase the likelihood of gestational diabetes, suggesting genetics play a role. Other risk factors include obesity, being overweight, less physical activity, and a history of cardiovascular diseases.
Prediabetes
Prediabetes can develop when your body doesn’t respond normally to insulin anymore. As your blood sugar rises, it increases the risk of developing type 2 diabetes later in life. Genetics, family history, being overweight, and insufficient exercise can encourage prediabetes.
Symptoms of Diabetes
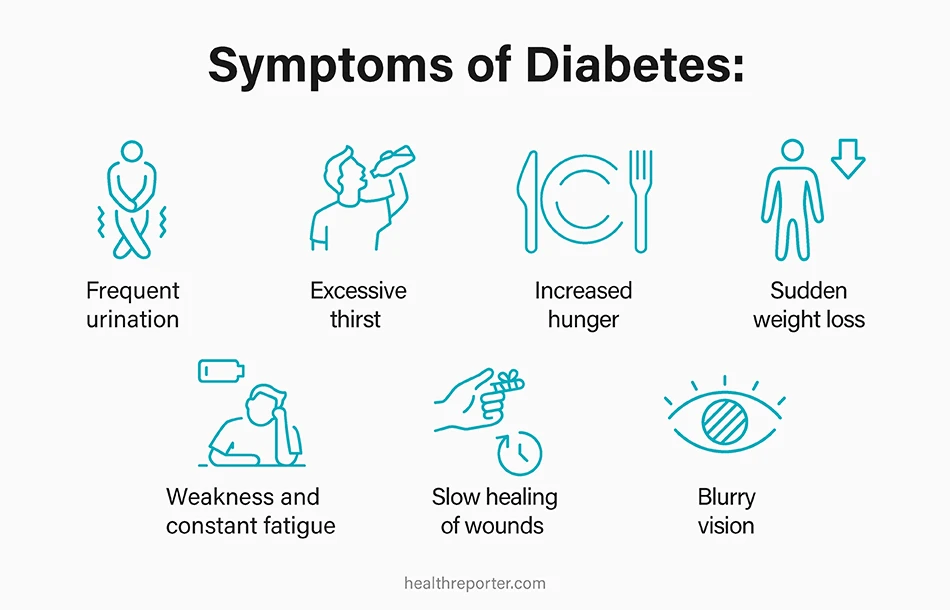
Spotting the symptoms of diabetes can help you take control of your health, mitigating the risk of complications. The symptoms don’t necessarily make you feel ill, so people often miss these early warning signs.
Some may indicate other issues, but it’s important to alert your doctor for a checkup.
#1 Frequent urination
Frequent urination, or polyuria, is one of the three P’s of diabetes, which describes three symptoms that often co-occur in undiagnosed diabetes. In adults, polyuria is quantified as passing more than 3–3.5 liters of urine per day, differing from the usual output of 1–2 liters.
#2 Excessive thirst
Polydipsia is another P of diabetes and describes abnormal thirst. You might feel thirsty throughout the day and find it impossible to quench your thirst despite adequate water intake. You’ll need to urinate more than usual to excrete the excess fluids.
#3 Increased hunger
The last medical term in the three P’s of diabetes is polyphagia, which means excess hunger. Again, this comes down to elevated blood sugar that can’t provide the energy you need. When food doesn’t give you energy, you might struggle to feel full regardless of your meals.
#4 Sudden weight loss
If you have diabetes, there is not enough insulin in your system. Without insulin, blood sugar cannot enter the body’s cells to convert into energy. With insufficient energy, the body burns fat and muscle to fuel itself instead. As a result, you might suddenly lose weight.
#5 Weakness and constant fatigue
Weakness and fatigue may occur when your body’s cells aren’t getting enough glucose from the blood to provide energy. Persistent fatigue can make it difficult to complete your usual tasks, and you might notice yourself falling asleep more often, such as after eating a meal.
#6 Slow healing of wounds
It’s estimated that impaired wound healing affects approximately 25% of all people with diabetes. This can happen because high blood sugar can impair immune function and stop nutrients from reaching your cells. Damage to nerves and vessels can also impair connective tissue healing.
#7 Blurry vision
Blurry vision links to diabetes because of changes in the eye’s refractive system. Elevated levels of blood glucose can alter fluid levels, causing the tissues in your eyes to swell. For some people with diabetes, blurry vision may trigger headaches – another possible sign.
Diabetes symptoms in women
Aside from the diabetes symptoms above, a few others can arise that affect men and women differently. The outcome can also differ between the sexes. For example, diabetes increases the risk of heart disease in both men and women, but it’s about four times higher in women and twice as high in men.
The symptoms affecting women specifically include:
- Yeast infections
- Changes in the menstrual cycle
- Sexual dysfunction
- UTIs
- Itchy and dry skin
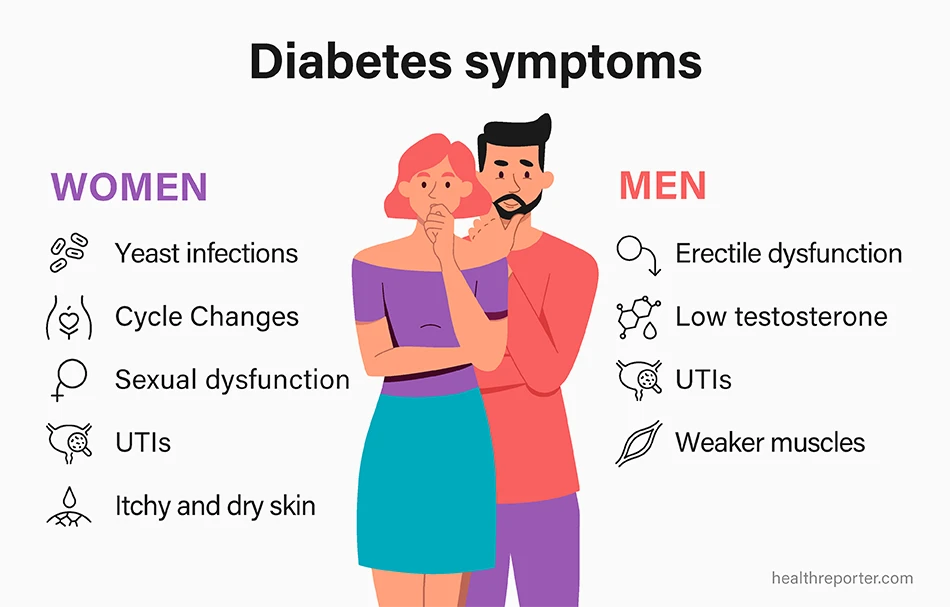
Diabetes symptoms in men
If you’re a man experiencing the following concerns alongside the typical diabetes symptoms, it may be a sign of diabetes. It’s best to schedule a visit with your doctor to determine or rule it out.
Symptoms affecting men include:
- Erectile dysfunction
- Lower testosterone levels
- UTIs
- Weaker muscles
How Is Diabetes Diagnosed?
Health professionals can diagnose diabetes using various diagnostic tests. These blood tests measure glucose levels in your bloodstream and are the only way to confirm if you have diabetes. Testing is straightforward and delivers results fairly quickly.
Doctors use one or more of the following tests to diagnose prediabetes, type 1 diabetes, and type 2 diabetes:
- A1c test
- Fasting blood sugar test
- Glucose tolerance test
- Random blood sugar test
Your doctor might then implement further tests to differentiate between types 1 and 2. These include autoantibody tests to spot substances that show your system is attacking itself and urine tests to check for ketone levels – two indicators of type 1 diabetes.
To diagnose gestational diabetes, the process requires a glucose screening test and glucose tolerance test, usually between 24 and 28 weeks into pregnancy.
Early detection is vital to gain control of diabetes. If you do have it, working with your healthcare team and attending regular checkups is essential.
How to Manage Diabetes? 7 Effective Strategies
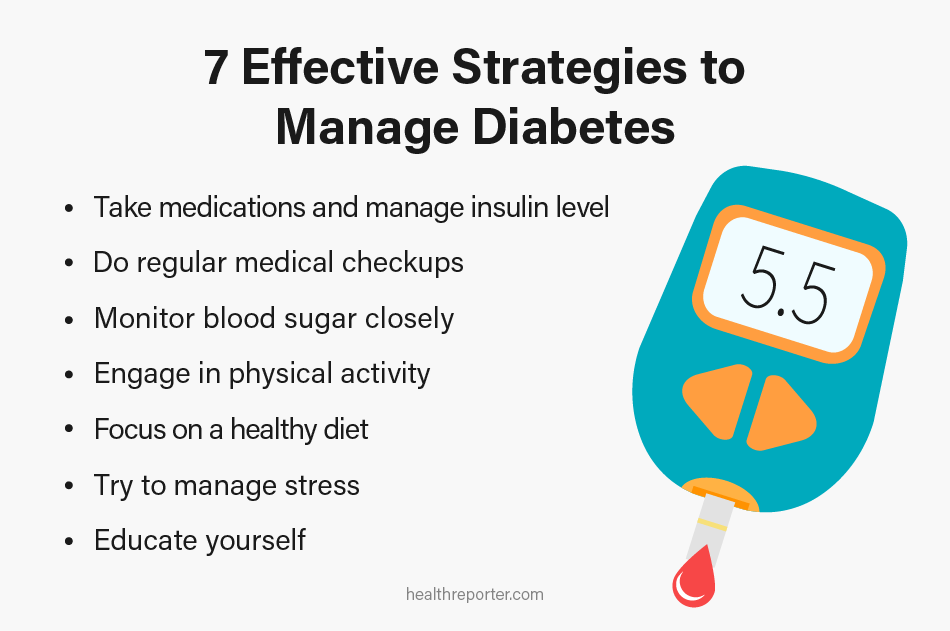
Whether you have type 1 diabetes, type 2 diabetes, or gestational diabetes, management is essential. Here are 7 ways to take care of yourself:
#1 Take medications and manage insulin level
Taking insulin and diabetes medication usually makes up part of diabetes management.
People with type 1 diabetes need insulin injections, while people with type 2 diabetes may need insulin or other prescription antidiabetic drugs. Metformin, for example, is often a doctor’s first recommendation for type 2 diabetes because it’s well-studied and well-tolerated.
Regardless of your medication, it’s vital to monitor your blood sugar levels to ensure the dosages are correct.
#2 Do regular medical checkups
Checkups are a regular part of a diabetes care plan. Visiting your doctor routinely ensures you manage your diabetes in the best way possible. They can examine your general health, look out for diabetes complications, and adapt your care plan accordingly.
Between doctor’s trips, it’s helpful to stay up-to-date with the latest advancements in diabetes management, such as apps with tools for tracking glucose, carb intake, and physical activity. You can always discuss things at your next appointment if you find something interesting.
#3 Monitor blood sugar closely
Routinely checking your blood sugar is vital as it allows you to see how your body responds to certain foods, the medication you take, and the different activities you partake in.
You will soon notice patterns and trends, making it easier to manage your diabetes and prevent high or low blood sugar levels. It also gathers more information you can share with your healthcare team to refine your treatment plan.
#4 Engage in physical activity
Keeping active is highly beneficial for diabetes because it supports weight management and improves insulin sensitivity, which in turn, aids glycemic control. Aim for the recommended 150 minutes per week, including your favorite activities like walking, jogging, and swimming.
#5 Focus on a healthy diet
Altering your diet is vital to balance your blood sugars. A healthy eating plan for diabetes means limiting sugary and processed foods and eating more whole foods, especially those high in fiber, like diabetes-friendly fruits, vegetables, and whole grains.
You might consider transforming your diet entirely, for example, by following a plant-based diet. The keto diet and fasting regimens also have advantages, particularly for weight control.
#6 Try to manage stress
Chronic stress can influence your health in several ways, including your blood sugar levels. Make your well-being a priority and keep stress at bay with proven stress management techniques, such as deep breathing exercises, meditation, stretching, and journaling.
Engaging in enjoyable activities can also promote relaxation, whether meeting a friend for coffee or attending an art workshop.
#7 Educate yourself
Educating yourself about diabetes can put you in a stronger position to manage your condition. The more you know, the better, and you can discover plenty of information from academic resources, workshops, and the people you meet at support groups.
After learning more about complications that may arise from diabetes later in life, you can create a self-care routine to help mitigate health problems. You could allocate time for footcare, activities to maintain a healthy weight, and schedule eye tests to maintain eye health.
Using a diabetes app is a good way to keep yourself informed about your condition, as many include educational content and tracking tools.
Lifestyle Tips for Living With Diabetes
Diabetes is a challenging disease, and it’s important to use the resources available for emotional and practical support, such as support groups and diabetes education programs. When you prioritize diabetes care, you can live a happy and healthy life.
Below are tips for social situations, traveling, and navigating challenges to help you manage diabetes.
Social situations
The best way to handle the social side of things is to communicate. Sharing your diagnosis with your friends, family, and colleagues can ensure you create a strong support network. You don’t have to face your diagnosis alone – let those closest to you be there for you.
At the same time, don’t expect people to understand your condition entirely. Instead, educate those around you about diabetes, as this will dispel misconceptions and equip them with the knowledge to support you better.
Diabetes typically requires you to alter your diet. You might feel that this disrupts your social life, but you can socialize without problems with little organization. For example, a simple phone call to communicate your dietary needs to the host can eliminate problems. You can even offer to bring your own dish to align with your requirements.
Traveling
When traveling, be sure to plan and pack your diabetes essentials. Consider carrying extra supplies in your hand luggage in case of delays or emergencies, such as insulin, medication, glucose monitoring equipment, and snacks to keep your blood sugar levels stable.
It’s helpful to carry something that informs others you have diabetes, like a diabetes card or a medical identification bracelet.
Challenges
Diabetes poses challenges, but you can prepare for these challenges in advance. For instance, you can tackle unexpected fluctuations in blood glucose by carrying a form of fast-acting glucose on you at all times, such as glucose tablets or a travel-size fruit juice.
Since stress, illness, infection, and other variables can trigger changes in blood sugar levels, make a plan of action to deal with these situations. Communicate with your doctor to make sure you know how to adjust your medication or insulin on these occasions if necessary.
Side Effects of Diabetes
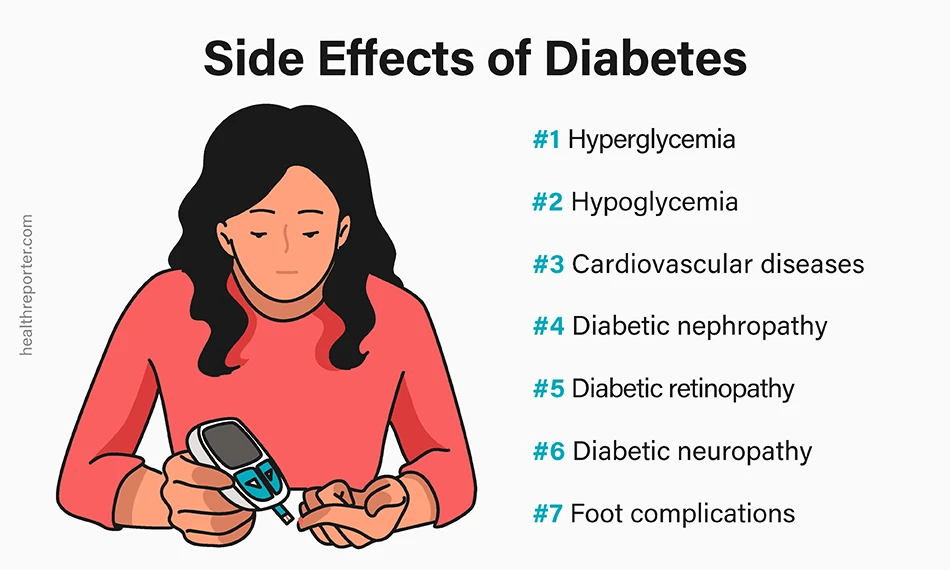
People with diabetes are at risk of severe side effects, as high blood sugar levels can cause significant damage to the body. After receiving a diagnosis, managing diabetes is a priority to mitigate further health problems.
Diabetes complications include:
#1 Hyperglycemia
Hyperglycemia is when your blood glucose levels get too high, with levels greater than 125mg/dL while fasting or 180mg/dL two hours after eating a meal. Losing weight, urinating frequently, and feeling thirsty, weak, and lethargic are warning signs.
These dangerously high levels can cause life-threatening complications, such as eye, heart, kidney, and nerve damage if ignored. People with diabetes can experience frequent episodes of hyperglycemia since there’s not enough insulin to control levels.
#2 Hypoglycemia
In contrast to hyperglycemia, hypoglycemia is when your blood sugar level drops below the healthy range. Low blood sugar can be just as harmful and is a common problem in people with diabetes, mostly those using insulin, glinides, or sulfonylurea to manage the condition.
As it presents an obstacle to attaining good glycemic control, recognizing the signs and accessing treatment is a key part of diabetes care, alongside balancing diabetes medication, diet, and exercise.
#3 Cardiovascular diseases
If you have diabetes, your chances of developing heart disease or a stroke double. This is because consistently high blood glucose levels can damage the blood vessels and nerves that keep your heart healthy.
In addition, having diabetes puts you at higher risk for high blood pressure, high cholesterol, and high triglycerides – all of which increase the risk of heart disease.
#4 Diabetic nephropathy
The heart isn’t the only organ under threat from diabetes.
Diabetic nephropathy is kidney disease triggered by both type 1 and type 2 diabetes. In the US, diabetes accounts for 30–50% of cases in patients with end-stage kidney disease. That said, diabetic nephropathy develops in just 30–40% of individuals with diabetes.
Interestingly, it is the diabetes complication of high blood pressure that contributes most to the disease, not high blood sugar. Nevertheless, damage to blood vessels in the kidneys from high blood sugar can prevent them from functioning normally.
#5 Diabetic retinopathy
Too much glucose in the bloodstream for a long time damages your retina, the back of the eye that converts light into electrical signals that trigger your brain to generate imagery. In other words, it is responsible for your vision. This condition is called diabetic retinopathy.
The retina relies on a steady blood flow from the central retinal artery and the short posterior ciliary arteries, but diabetes gradually damages these vessels. It can take years for diabetic retinopathy to affect your sight, but it can eventually leave you blind if you neglect treatment.
#6 Diabetic neuropathy
Another complication is diabetic neuropathy, which is nerve damage. Too much glucose can injure different kinds of nerves in your body, but it primarily affects those in the legs and feet. Depending on the neuropathy type, you might feel numbness and tingling or pain and sensitivity.
#7 Foot complications
Foot problems often result from neuropathy. With damage to the nerves in your feet, tingling and burning or stinging sensations, or even a complete loss of feeling can occur. In this case, you might miss injuries to your feet that you’d ordinarily spot because you don’t feel pain.
It can take a while for your feet to mend, too. Poor blood flow can mean slow healing sores and wounds as blood vessels harden. The body’s attempt to heal itself, coupled with impaired blood flow, can cause fluid to pool in the feet and ankles, and you may develop swollen feet.
To mitigate severe complications, good footcare remains an integral part of diabetes management.
FAQs
Peeing a lot, excessive thirst, excessive hunger, weight loss, and fatigue are some signs that may indicate diabetes mellitus. Many people don’t know they have diabetes because they don’t feel sick. Only a blood test can confirm if you have it.
Early signs of diabetes typically include the three p’s: polydipsia, polyuria, and polyphagia, which correspond to excessive hunger, thirst, and urination. Other signs include fatigue, blurry vision, unexplained weight loss, slow-healing wounds, and numb or tingling feet.
Diabetes is a chronic disease driven by an increase in blood glucose. Type 1 diabetes is an autoimmune disease affecting the insulin-producing cells in the pancreas. In contrast, type 2 diabetes is a problem with the body’s ability to handle the insulin produced.
Diabetes can eventually result in death. According to the Centers for Disease Control and Prevention, it is the 8th leading cause of death in the US. Cardiovascular diseases and cancer are the most common cause of diabetes-related deaths in types 1 and 2.
What does diabetes feel like?
People don’t necessarily feel diabetes but can experience symptoms that indicate the disease. People with diabetes mostly feel tired, very thirsty, and need to urinate more than usual. They might experience polyphagia, too, which means feeling hungrier.
A Word From Our MD
Diabetes is chronic, life-threatening, and demands intervention. Book an appointment with your doctor if you suspect that you have diabetes symptoms, like the three p’s and sudden weight loss. Getting your blood sugar tested is the only way to find out.
Family history and genetics are risk factors for type 1 diabetes, while lifestyle habits are common risk factors for type 2 diabetes, such as smoking and being overweight or inactive.
Conclusion
There’s no cure for diabetes, regardless of whether you have type 1 or type 2 diabetes.
However, you can control it by managing your blood glucose levels through medication and lifestyle modifications. Gestational diabetes usually goes away when the baby arrives. But sometimes, pregnancy may uncover existing diabetes that requires long-term treatment.
















































 Select your language:
Select your language: 








