Comparison of the Ketogenic Diet and Fasting for People With Diabetes

Health Reporter has been looking at the effectiveness and safety of the ketogenic diet and intermittent fasting (IF) for those who suffer from type 1 or type 2 diabetes.
It is currently estimated that 10.5% of the adult (over 18 years old) US population has a form of diabetes – that’s over 34 million people. This number rises to 13% when looking at the population as a whole. Diabetes is growing at an alarming rate globally, with 1 in 10 people said to be suffering.
It is also estimated that the prevalence of diabetes in adults worldwide is over 300 million, and it will increase by 55% by 2035.
Key findings:
- Studies found that keto improved insulin sensitivity by 75%.
- A study of 349 people with type 2 diabetes found that people on keto lost an average of 26.2 pounds over two years.
- A review of 12 studies of patients following some form of IF showed insulin sensitivity improved, regardless of the type of fasting protocol they followed.
- Researchers discovered that routine fasters had a 45% lower mortality rate than non-fasters during the follow-up period.
- Various studies show that fasting can help lower blood pressure, reduce cholesterol, control diabetes, and reduce weight.
What Is Diabetes?
Diabetes is a chronic (long-lasting) health condition that affects how your body turns food into energy.
Most of the food you eat is broken down into sugar (also called glucose) and released into your bloodstream. When your blood sugar goes up, it signals your pancreas to release insulin. Insulin acts like a key to letting the blood sugar into your body’s cells for use as energy.
What is the difference between type 1 and type 2 diabetes?
Most people know there are two main types of diabetes, but not everyone understands the difference between them.
In type 1 and type 2 diabetes, blood sugar levels can get too high because the body doesn’t produce insulin (a hormone that regulates blood sugar) or does not utilize insulin properly. Though the problem is essentially the same in both types, they have different causes and treatments.
The main difference between the two types of diabetes is that type 1 diabetes is a genetic disorder that often shows up early in life, and type 2 is lifestyle-related and develops over time. If you have type 1 diabetes, your immune system is attacking and destroying the insulin-producing cells in your pancreas.
Managing Weight Loss – Keto vs. Fasting
Both the keto diet and variations of fasting diets have improved the overall health of people with diabetes. Below, we will compare the two and see which diet leads to greater success, starting with the keto diet.
The ketogenic diet can help lose excess fat, which is closely linked to type 2 diabetes. A study of 349 people with type 2 diabetes found that people on keto lost an average of 26.2 pounds (11.9kg) over two years.
People with type 2 diabetes are often advised to control their intake of carbohydrates because they can turn into sugar and cause blood sugar spikes when consumed in large amounts. People with type 2 diabetes often find that their blood sugar improves when they start keto. This is because keto lowers blood sugar levels.
Keto also usually dramatically reduces the need for medications, especially insulin. Studies found that keto improved insulin sensitivity by a whopping 75%.
Another study looked at the effect of the ketogenic diet on glycemic control, insulin resistance, and lipid metabolism in patients with type 2 diabetes and found that after keto diet intervention, in terms of glycemic control, the level of fasting blood glucose decreased by 23.22mg/dL (1.29mmol/L) on average.
It was also found that, on average, total cholesterol fell by 0.33%. In addition, patients’ weight decreased on average by 8.66%, waist circumference by 9.17%, and BMI by 3.13%.
The study concluded that the keto diet had a therapeutic effect on glycemic and lipid control among patients with type 2 diabetes and significantly contributed to their weight loss.
Type 2 diabetes is generally regarded as an irreversible chronic condition. A study tested the potential durability of this normalization because a very low-calorie diet such as fasting can bring about an acute return to normal glucose control in some people with type 2 diabetes. The underlying mechanisms were defined.
Weight fell (216lbs to 185lbs) and remained stable over 6 months, with the study also finding that a robust and sustainable weight loss program achieved continuing remission of diabetes for at least 6 months in the 40% by achieving fasting plasma glucose of <126mg/dL (7mmol/L). This suggests that type 2 diabetes is a potentially reversible condition.
Further studies indicate that intermittent fasting effectively reduces body weight, decreases fasting glucose, decreases fasting insulin, reduces insulin resistance, decreases leptin levels, and increases adiponectin levels.
Some studies found that patients could reverse their need for insulin therapy during therapeutic intermittent fasting protocols with supervision by their physician.
Current evidence suggests that intermittent fasting is an effective non-medicinal treatment option for type 2 diabetes. More research is needed to determine the effects of intermittent fasting on weight loss.
Physicians should consider educating themselves regarding the benefits of intermittent fasting. People with diabetes should consult their physician before beginning an intermittent fasting regimen to ensure proper medication supervision and adjustment during fasting periods.
So based on the research above, the keto diet is the recommended diet of choice for people who have diabetes. It allows users to burn excess fat, which is closely linked to type 2 diabetes. It has also been shown to reduce high cholesterol levels and help manage blood sugar.
While fasting also has some positive influence on diabetes, the benefits of the keto diet simply outweigh those of fasting diets.
Managing Insulin Sensitivity – Keto vs. Fasting
Insulin sensitivity refers to how sensitive the body’s cells respond to insulin. High insulin sensitivity allows the body cells to use blood glucose more effectively, reducing blood sugar. Some lifestyle and dietary changes may help improve this sensitivity.
Insulin is a hormone that helps the body control the level of sugar, or glucose, in the blood. Insulin sensitivity varies between people and can change according to various lifestyle and dietary factors.
A person with low insulin sensitivity also has insulin resistance, which affects about 38% of adults in the United States. People with insulin resistance have a higher risk of developing type 2 diabetes.
Improving insulin sensitivity and reducing insulin resistance may benefit those who have or are at risk of type 2 diabetes.
Based on a meta-analysis that systematically reviewed 13 relevant studies, it was found that the ketogenic diet can not only control fasting blood glucose and reduce glycosylated hemoglobin but also improve lipid metabolism.
Additionally, a ketogenic diet can reduce BMI and body weight. Therefore, the ketogenic diet may be used as part of the integrated management of type 2 diabetes.
With the keto diet, during the ketogenesis, the sensitivity of the insulin receptor is promoted; therefore, the keto diet not only ensures the supply of essential nutrients but also maintains a negative balance of energy and reduces the fluctuation and reduction of insulin secretion caused by reduced carbohydrate intake as well, which eventually leads to improved insulin sensitivity.
As for fasting, popular intermittent fasting protocols range from fasting a few hours each day, fasting every other day, or doing a modified fast a few days of the week. Studies conducted on humans show the best type of IF schedule is the one that works for you.
A 2018 study showed an 18:6 fasting protocol (fasting for 18 hours of the day and eating for 6) improved insulin sensitivity in men with prediabetes. Another smaller study of patients with diabetes showed that various schedules of 24-hour fasts were beneficial to reducing insulin resistance. This review of 12 studies of patients following some form of IF showed insulin sensitivity improved, regardless of the type of fasting protocol they followed.
According to Jason Fung MD, founder of “The Fasting Method,” the most important aspect of an IF diet is that fasting lowers insulin levels. Your most effective strategy to fast for increased insulin sensitivity will be the form of intermittent fasting that matches your lifestyle and is simplest to sustain.
Five weeks of fasting improved insulin levels, insulin sensitivity, cell responsiveness, blood pressure, and oxidative stress levels in men with prediabetes – even though food intake was matched to the control arm, no weight loss occurred. In one trial, 24 hours of fasting decreased insulin sensitivity the following morning by 54%.
This comparison is much closer, but we’re giving the edge to fasting. When looking to manage or even improve insulin sensitivity, more research has been conducted into the positives of fasting diet types.
Studies suggested that insulin sensitivity improved each time regardless of which fasting protocols were chosen. The keto diet is also a safe way to manage your diabetes, specifically insulin levels, but fasting takes first place.
Improving Cholesterol – Fasting vs. Keto
When analyzing the keto diet’s influence on improving cholesterol, one study of 83 obese patients (39 men and 44 women) with a body mass index greater than 77 lbs/m(2) and high glucose and cholesterol levels were selected.
The body weight, body mass index, total cholesterol, and fasting blood sugar levels were determined before and after the administration of the ketogenic diet. Changes in these parameters were monitored after 8, 16, and 24 weeks of treatment.
The patients’ weight and body mass index decreased significantly (p < 0.0001). The total cholesterol level decreased from week one average of 97.2mg/dL (5.4mmol/L) to the week 24 average of 84.5mg/dL (4.7mmol/L). HDL cholesterol levels significantly increased, whereas LDL cholesterol levels significantly decreased after treatment.
The present study shows the beneficial effects of a long-term ketogenic diet. It significantly reduced the body weight and body mass index of the patients. Furthermore, it decreased the level of cholesterol and blood glucose and increased the level of HDL cholesterol.
When looking at the influence of fasting diets on improving cholesterol levels, regular fasting can decrease your low-density lipoprotein, or “bad,” cholesterol. It’s also thought that fasting can improve the way your body metabolizes sugar. This can reduce your risk of gaining weight and developing diabetes, both risk factors for heart disease.
A 6-week quasi-experimental (non-randomized) clinical trial was conducted on participants with low HDL (<40mg/dL for men and <50mg/dL for women). Participants of the control group were recommended not to change their diet.
The intervention group was recommended to fast for 12h during the daytime, three times per week for 6 weeks. Pulse rate, blood pressure, body weight, waist circumference, serum lipid profile, and blood glucose levels were measured at baseline and after 6 weeks.
A total of 40 participants were enrolled in the study (20 in each group), while 35 (20 control and 15 intervention) completed the trial and were included in the study’s data analysis.
Body measurements, including body weight, BMI, and waist circumference, showed significant interaction effects (p < 0.001), indicating larger reductions in the IF group than in the control group. Significant interaction effects were also observed for total (p = 0.033), HDL (p = 0.0001), and LDL cholesterol (p = 0.010) with larger improvements in the IF group.
Another close call, but the keto diet wins this round. More extensive studies have been tested, and the results are clearly in favor. The keto diet is excellent at lowering cholesterol levels, as well as more significant improvements in BMI and overall weight, making it a safer and more sure option than fasting, which itself has been shown to improve cholesterol levels, but less research has been carried out to support it.
Improving Inflammation – Keto vs. Fasting
While the research into keto and inflammation is limited, one study found that a 40-year-old woman with type 2 diabetes mellitus, obese (220lbs), on insulin (80 units), was under treatment for unstable proliferative diabetic retinopathy with extramacular tractional retinal detachment (TRD) in the left eye.
At 1-year follow-up, she developed a progression of TRD involving the macula in the left eye, for which she was advised surgery. She did not follow up for 6 months, during which time she had adopted a coconut oil-rich ketogenic diet.
She reported losing 55lbs along with the reversal of diabetes. During the 2-year follow-up visit, it was found that there was complete resolution of macular detachment due to TRD in the left eye with stable vision. This was attributed to the impactful ketogenic diet.
As for fasting diets’ impact on inflammation, one study found that intermittent fasting (IF) prevented diabetes-induced clock dysfunction and the formation of acellular capillaries in the retina.
This effect was not due to the restoration of glucose levels. Instead, IF affected the circadian rhythms of inflammatory monocytes. During the fasting period of the IF regimen, monocytes were depleted by 50% from circulation independently of the status of diabetes or time.
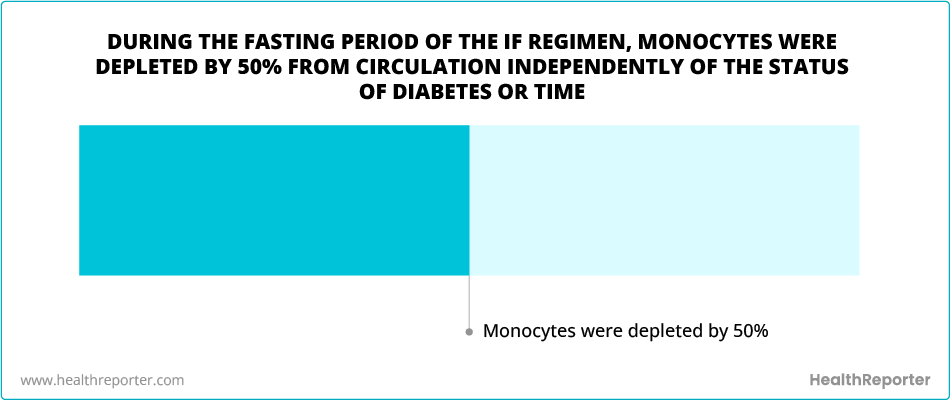
It was concluded that the availability of nutrients significantly governs the behavior of monocytes and drives inflammation. The prevention of diabetic complications is associated with the reduced inflammation observed during the fasting state of the IF treatment.
Overall, there is very little research exploring the effects of both keto and fasting diets when looking to improve inflammation. So we have marked this down as a draw, as both have loose examples of success, but until further research is carried out, the effects are seen as equals.
Heart Disease – Keto vs. Fasting
The keto diet is associated with higher HDL levels, a lipoprotein known as good cholesterol that is associated with decreased risk of heart disease. Despite these promising effects, the keto diet is also associated with higher levels of LDL or bad cholesterol, which increases cardiovascular risk.
The keto diet also has a powerful effect on lowering blood sugar. This diet has been shown in multiple studies to decrease blood sugar as measured by hemoglobin A1C levels and reduce the need for diabetes medication.
However, people taking medication for diabetes should not start this diet without speaking to their healthcare provider first. Medication adjustment may be needed to avoid dangerously low drops in blood sugar.
However, there are concerns about the adverse effects on heart health with the ketogenic diet. Many studies have shown the association of keto diets with increased LDL (bad cholesterol), but this finding is not consistent in all studies. Keto diets high in saturated and trans fats seem to be responsible for the increased LDL levels.
To minimize this risk of heart disease while on a ketogenic diet, it is advised to minimize processed foods high in saturated and trans fats and instead choose plant-based foods with higher unsaturated fat content.
What about fasting and heart disease?
According to new studies, regular fasting is associated with lower rates of heart failure and a longer life span.
In one study, researchers zeroed in on how fasting impacts life span. About 2,000 people who had undergone a cardiac catheterization procedure were followed for an average of 4.4 years, including 389 “routine fasters” who had been fasting regularly for at least 5 years.
After adjusting for various factors, researchers discovered the routine fasters had a 45% lower mortality rate than the non-fasters during the follow-up period.
Another fasting study used the same patient data to see how routine fasting affects heart failure and heart attacks. After adjusting for various factors, there was no significant difference in heart attacks, but routine fasters had a 71% lower rate of heart failure than non-fasters.
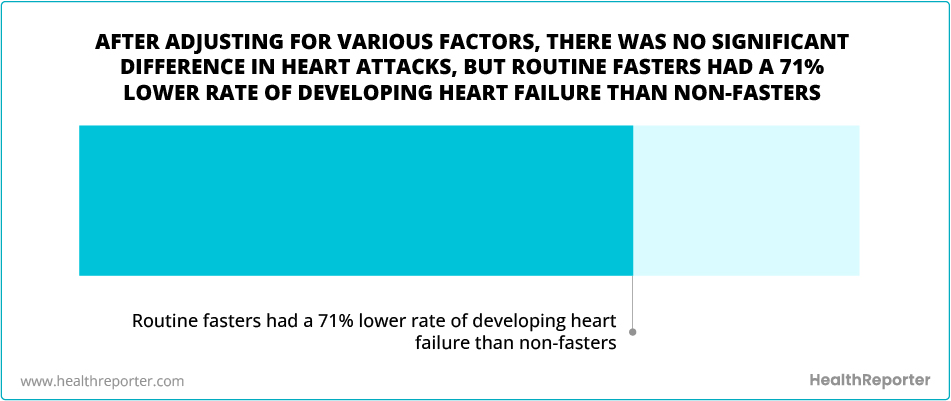
So fasting nicks this one for us. While there has been significantly more research into the keto diet and heart health, the documented potential risks and side effects are riskier than fasting. More research needs to be carried out to highlight any potential dangers fasting holds for people with diabetes, but going on the currently available studies, fasting is the winner.
Blood Pressure – Fasting vs. Diabetes
The ketogenic diet has been proposed to be an effective lifestyle intervention for metabolic syndrome in recent years.
Although the beneficial effects on weight loss and glucose metabolism seem to be well established, the impact of a prolonged KD on the ability to perform different types of exercise and the influence of KD on blood pressure (BP) levels, both in normotensives and in hypertensives, are not so well understood.
The mechanisms by which keto may promote fat loss include appetite suppression, increased energy burn, and increased fat burning due to low insulin levels.
So it would seem that keto has the potential to help with high blood pressure by fighting the hypertension risk factors of obesity and diabetes.
There may be cases where a keto diet would pose a risk to blood pressure; for instance, a dirty keto diet would be short on potassium (from vegetables) to counter the high sodium load from salty processed meat.
Too much sodium without enough potassium will raise blood pressure, while too little sodium can also raise blood pressure. When you don’t consume enough sodium, your body releases a sodium-retaining, blood-pressure-raising hormone called aldosterone.
As for fasting, research shows that fasting can help lower blood pressure, reduce cholesterol, control diabetes, and reduce weight.
Four of the major risks for heart disease are high blood pressure, cholesterol, diabetes, and unhealthy weight, so there’s a secondary impact. If those can be reduced, you can reduce the risk of heart disease.
In a 2020 study in the journal Cell Metabolism, intermittent fasting helped women with metabolic syndrome. This is a group of symptoms including high blood pressure, high blood sugar, excess abdominal fat, and abnormal blood fat levels that raise the risk of heart disease and diabetes.
When the women only ate within a 10-hour window during the day, they had lower blood pressure, better cholesterol, and fewer blood sugar spikes.
Research also shows that intermittent fasting lowers chronic inflammation. Inflammation can damage blood vessels and increase the risk of heart attacks and strokes.
Yet again, we think fasting has done enough to secure this one. There have been countless studies demonstrating the positive effects of fasting diets on heart health, from improvements in blood pressure, heart disease, and inflammation to reducing the risk of heart attacks and strokes. And while the keto diet has shown promising results as well, its potential side effects tip this in favor of fasting.
So What Is the Best Diet for People With Diabetes?
It was very close between the two, but here are the results:
Managing weight loss – fasting
Managing insulin sensitivity – keto
Managing cholesterol – keto
Improving inflammation – draw
Heart disease – fasting
Improving blood pressure – fasting
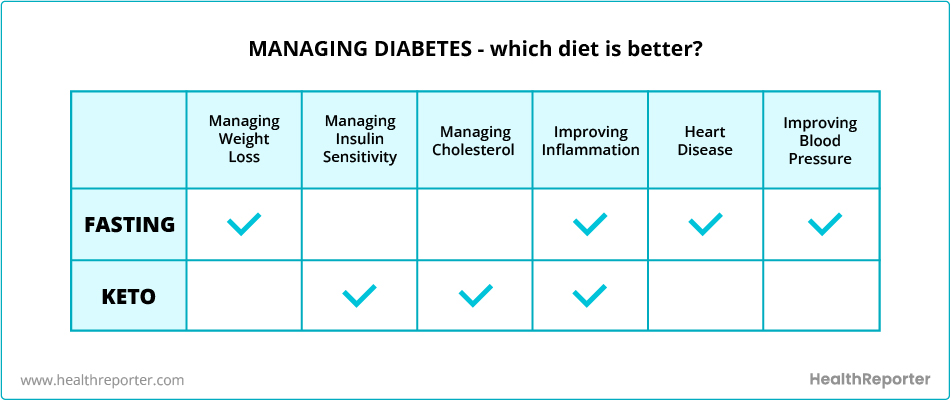
We think this is a 3:2 victory for fasting, and overall, we think this is a fair result. Both diets come with a host of positive benefits for those who have diabetes, but due to the volume of research supporting fasting, and the potential risks highlighted above with keto, the former is the Health Reporter recommendation for people with diabetes.
You should always consult your doctor and iron out any potential risks to your health before participating in any diet.
Sources:
CDC, Diabetes Atlas, NCBI, PubMed, PubMed 2, PubMed 3, PubMed 4, PubMed 5, Diabetes Journals, NCBI 2, Medical News Today, NCBI 3, NCBI 4, PubMed 6, Mayo Clinic, Frontiers in Nutrition, PubMed 7, Arvo Journals, Academic OUP, Diabetes Journals 2, Lipid Journal, AHA Journals, AHA Journals 2, Carb Manager, Cleveland Clinic, Cell 1, Cell 2
















































 Select your language:
Select your language: 








