Here’s Why the Twitter Insulin Scandal Is More Important Than It Seems

There have been a lot of scandals on Twitter recently. Some of them are forgotten as quickly as they appear, while others reflect deep societal crises that can no longer remain in the shadows. Why did one of the many fraudulent tweets cause such a broad public outcry? Let’s figure it out.
Insulin, Elon Musk, and Eli Lilly
A few weeks ago, Elon Musk introduced the Twitter Blue subscription, which allows users to buy a blue checkmark for $8 to verify their account for authenticity.
Among others who liked the update, there were naturally scammers. One of them decided to impersonate the official page of the pharmaceutical company Eli Lilly, on which he posted the following message:

Although the fake account was soon suspended, it had already done the damage: in a matter of hours, the shares of Eli Lilly began to lose value. Worried shareholders decided it was a real company statement and sold shares in a rush.
According to Forbes, the pharmaceutical giant lost $16 billion of the company’s market value.1
The incident forced Twitter to put the Twitter Blue subscription on hold for review. Eli Lilly had to apologize in their official account, which has only fueled the fire among users. The scandal flared up with renewed vigor, but now regarding the cost of insulin.
The Long-Festering Debate About Insulin Prices in the US
After the tweet about free insulin, many Twitter users began criticizing the pharmaceutical company for profiting from people with diabetes. One of the first to react was the junior US senator Bernie Sanders.2
He states the problem is not about the “free insulin” tweet but the significant increase in the price of insulin in the country:
“Eli Lilly should apologize for increasing the price of insulin by over 1,200% since 1996 to $275 while it costs less than $10 to manufacture. The inventors of insulin sold their patents in 1923 for $1 to save lives, not to make Eli Lilly’s CEO obscenely rich.”
Others have expressed a similar point of view:
“What you should *actually* apologize for is price gouging life-saving insulin,” tweeted Qasim Rashid, Chicago-based human rights lawyer.3
Later, the discussions left the confines of Twitter and began to increasingly flicker in the media, as well as expressed through the actions of civil society.
“Fake Eli Lilly might be offering something closer to the truth than real Eli Lilly,” Peter Maybarduk, the nonprofit Public Citizen representative, told AFP.
On World Diabetes Day, which took place on November 14, advocacy groups, including Public Citizen, T1 International, and others, sent a letter to Congress demanding a stop to insulin price-gouging.4
The company’s share price never recovered from the fall, and that’s the price of online misinformation. However, the scandal has also triggered a new wave of discussions about public health issues. One can only hope that these debates can lead to tangible results.
Status Quo on the Insulin Market. Can the Situation Be Changed Quickly?
A quarter of Americans who take insulin have to miss injections or take insufficient doses, putting themselves at risk of severe complications.5 For more than 14% of people using insulin in the US, spending on it takes at least 40% of their income.6
So why is insulin so expensive in the US? The main reason for the high cost is patents for original drugs. US law provides 20 years of patent exclusivity, but this period can be extended with secondary patents. It turns out that companies may hold patents for an incredibly long time.
Moreover, only three companies hold patents for insulin preparations in the US: Eli Lilly, Sanofi, and Novo Nordisk (they also control 96% of the global market).
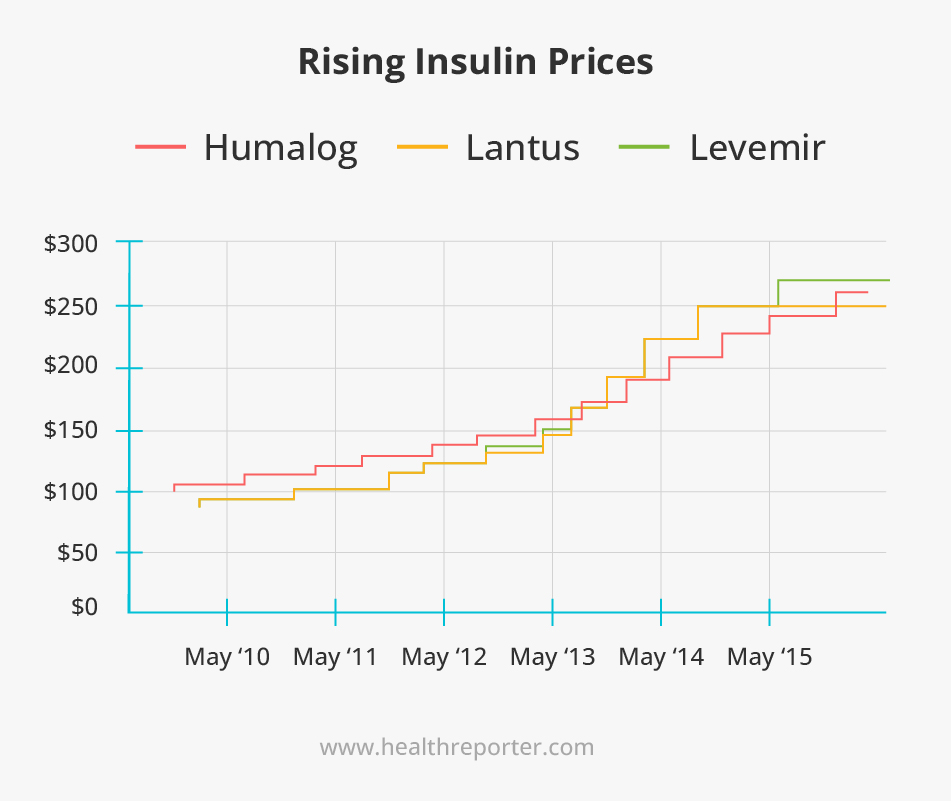
From 2010 to 2015, the price of Lantus (made by Sanofi) went up by 168%, the price of Levemir (made by Novo Nordisk) rose by 169%, and the price of Humulin R U-500 (made by Eli Lilly) soared by 325%.7
Unlike many other countries, the US also gives pharmaceutical companies a free hand in setting prices.
But why does a drug created a hundred years ago not have generics available? A drug patent prohibits the creation of copies of it, that is, generics. But the situation is different with drugs produced using biotechnology.
An analog of a biotech drug is called a biosimilar. Creating it is much more complicated than a generic drug – you have to modify bacteria from scratch – and even harder to register. And because of the complex system within the market, the situation cannot be changed quickly.
So, many people with diabetes in the US are getting sick or even dying from their inability to access insulin.
Future of Diabetes Therapy
There is hope that cutting-edge advances in insulin therapy may soon offer people with diabetes new ways to treat the disease.
There are three main types of insulin in use today, which differ in onset, peak, and duration of action:
- Fast-acting
- Intermediate-acting
- Long-acting
However, there is currently no insulin preparation that perfectly mimics the physiological action of the hormone in the body. So researchers continue to look for better options – let’s take a look at a few promising ones!
Smart insulins: After injection, they adapt to the level of sugar
The availability of short-acting and long-acting insulins has greatly simplified the management of diabetes. They allow most patients to regulate their sugar metabolism optimally.
However, people with diabetes who are on insulin therapy should measure their blood sugar levels before meals, calculate the required insulin dose, and then administer it.
Thus, the idea is to create a depot of insulin in the body, from which the hormone is released into the blood exactly when it is needed – that is when blood sugar levels rise. These insulins are also called glucose-sensitive.
So far, a prototype that reacts to fructose has been created. Scientists are confident that getting a working version sensitive to glucose will not be a problem.
Immunotherapy instead of insulin
Insulin and its analogs still do not provide satisfactory glycemic control in a significant proportion of patients with type 1 diabetes. Under these conditions, scientists hope for immunomodulatory therapy, which can ensure the preservation of the function of the patient’s beta cells in the preclinical stages of the disease.
This approach has demonstrated its safety in small clinical trials.8 According to scientists, immunotherapy can be used for 5–10 years without contraindications.
Insulin delivery in non-injectable ways
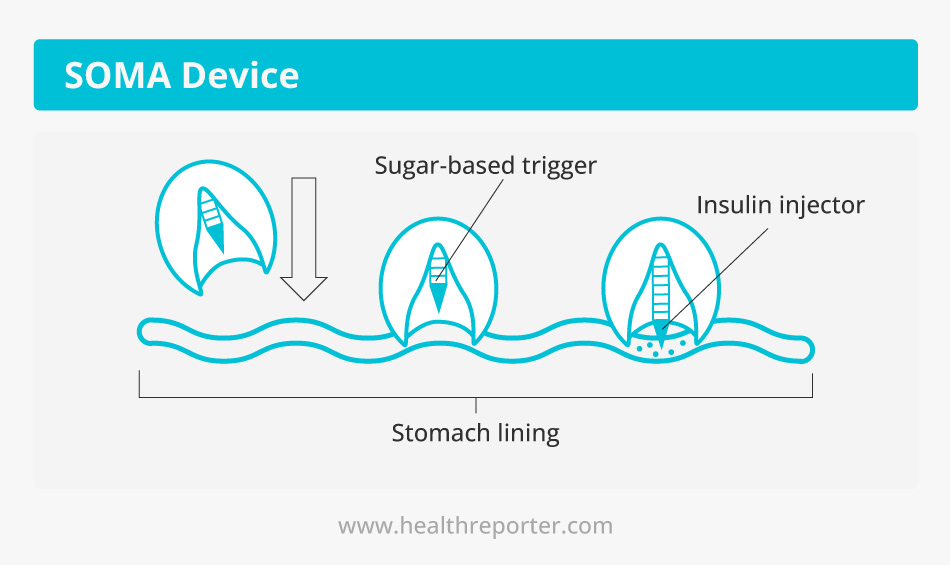
US scientists have created a tiny SOMA device that delivers therapeutic agents, including insulin, directly to the gastric mucosa.
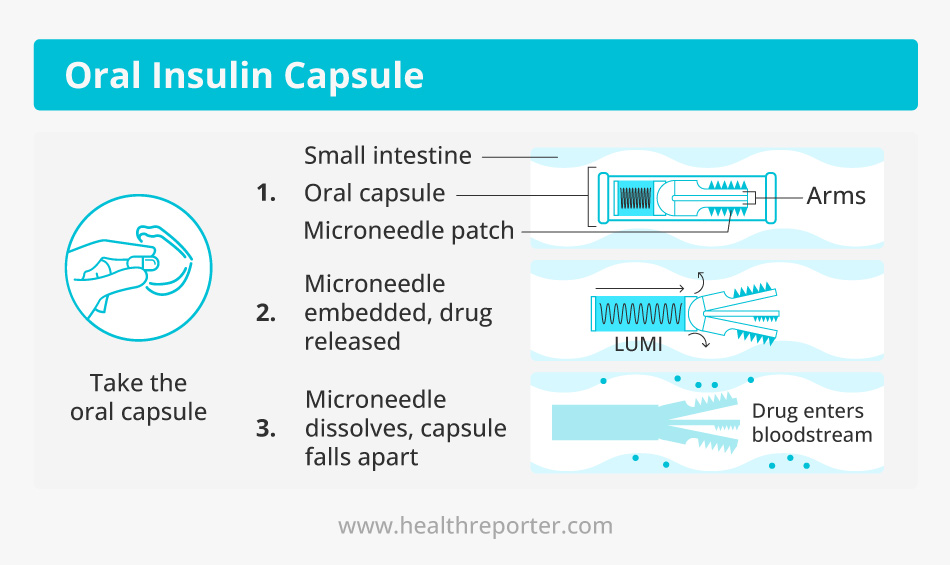
Besides, Oramed Pharmaceuticals has been successfully developing the oral insulin capsule ORMD-0801 for some time.
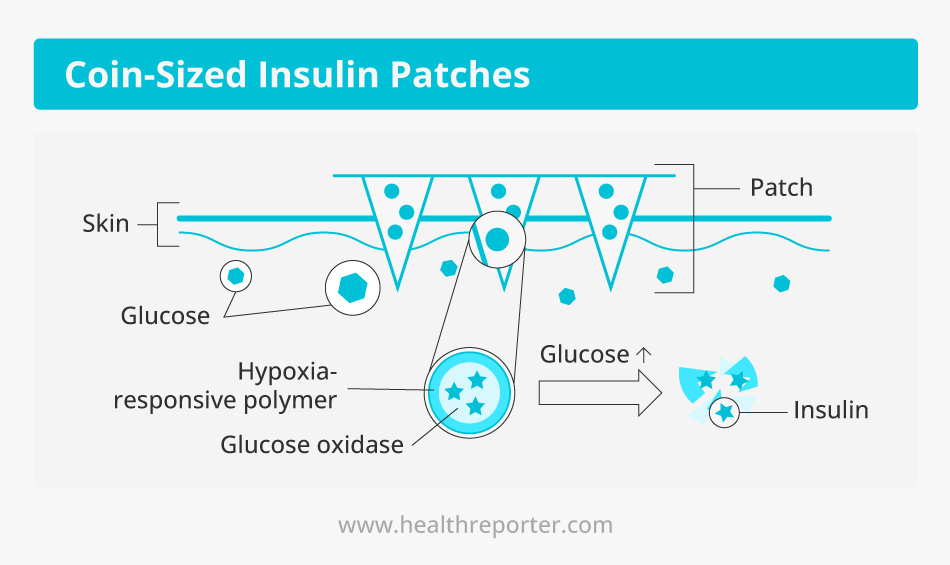
Coin-sized “smart” insulin patches have also shown promising results in recent animal studies.
Among other innovations
- New types of insulin have also been developed, such as glargine (insulin for subcutaneous injection), aspart, and 75/25 lispro mixture, which are very fast-acting insulins.
- A new ultra-long-acting basal insulin that can be administered weekly is in the early stages of development.
- Moreover, scientists are developing twincretins (when drugs of different effects are combined in one tablet).
These innovations cannot but give hope to make life as comfortable as possible for people with diabetes. Are we on the threshold of a beautiful future? It’s hard to say yet. But what is important now is to make all scientific achievements available to as many patients as possible.
Conclusion
The high price of insulin in the US is one of the many issues that cannot be ignored. Otherwise, it will keep getting on the agenda in the most diverse forms (such as a Twitter scandal). This will start generating new waves of debate, but these waves also tend to subside.
Should we wait for the next trigger? Or a new scientific discovery that will make insulin more affordable? Anyway, we must remember that the time our reasoning takes can cost lives. So, profound systemic changes in the American healthcare system must be made as soon as possible.
Sources
- Fake Eli Lilly Twitter Account Claims Insulin Is Free, Stock Falls 4.37%:
https://www.forbes.com/sites/brucelee/2022/11/12/fake-eli-lilly-twitter-account-claims-insulin-is-free-stock-falls-43/?sh=648d6ff241a3
- Bernie Sanders. (2022). Twitter:
https://twitter.com/BernieSanders/status/1591167058917478400?s=20&t=OpgyN_IRaFrSYNd07V7A1w - Cost-Related Insulin Underuse Among Patients With Diabetes:
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2717499?_ga=2.80924754.415518978.1668435891-1518137624.1668435891 - Catastrophic Spending On Insulin In The United States, 2017–18 | Health Affairs:
https://www.healthaffairs.org/doi/10.1377/hlthaff.2021.01788 - Insulin: A life saving drug too often out of reach:
https://diabetescaucus-degette.house.gov/sites/diabetescaucus.house.gov/files/Congressional%20Diabetes%20Caucus%20Insulin%20Inquiry%20Whitepaper%20FINAL%20VERSION.pdf - Metabolic and immune effects of immunotherapy with proinsulin peptide in human new-onset type 1 diabetes:
https://www.science.org/doi/10.1126/scitranslmed.aaf7779 - CDC 2022 National Diabetes Statistics Report:
https://nationaldppcsc.cdc.gov/s/article/CDC-2022-National-Diabetes-Statistics-Report#:~:text=The%20Centers%20for%20Disease%20Control,prediabetes%20in%20the%20United%20States
















































 Select your language:
Select your language: 








